 While recent headlines claim that rising drug prices can be easily addressed through government intervention, the procedures involved with government use of patented technologies are complex and often misunderstood. In addition to owning and practicing a vast portfolio of patents, the government has the power to procure and use patented technologies—including pharmaceutical medicines—in limited circumstances without specific authorization, license, or consent. But despite established mechanisms for government use of intellectual property, some advocates are now promoting an unprecedented and expansive interpretation of procurement that would deprive patent owners of their rights and threaten pharmaceutical innovation.
While recent headlines claim that rising drug prices can be easily addressed through government intervention, the procedures involved with government use of patented technologies are complex and often misunderstood. In addition to owning and practicing a vast portfolio of patents, the government has the power to procure and use patented technologies—including pharmaceutical medicines—in limited circumstances without specific authorization, license, or consent. But despite established mechanisms for government use of intellectual property, some advocates are now promoting an unprecedented and expansive interpretation of procurement that would deprive patent owners of their rights and threaten pharmaceutical innovation.
Today, escalating health care costs raise concerns from lawmakers on both sides of the political aisle. The U.S. pharmaceutical market alone was $333 billion in 2014.[1] Critics cite the escalating cost of certain specialty drugs as a leading cause of the high cost of health care, and some argue that price disparities have a disproportionate effect on certain groups. Accordingly, it has been argued that the federal government already has a responsibility and the necessary legal tools to combat the high price of drugs, e.g., through its procurement procedures. Yet combating disproportionate drug prices through government procurement should be a carefully considered process and not one based on misrepresentations of the history and rationale behind federal procurement procedures.
Federal Government Procurement Overview
The U.S. government oversees a vast and complex procurement system, including the General Services Administration (e.g., real estate, property, and services), the Federal Acquisition Regulation (FAR) system, and vast federal contracting. In sum, the annual federal budget will exceed $4.4 trillion in 2019.[2] Advocates note that the federal government spent nearly $1.1 trillion on health care alone in 2018.[3] In the health care sector, the federal government’s role is also exemplified by the following categories of activity: the direct purchasing of pharmaceutical through federal agency programs including, the Veterans Health Administration, Department of Defense, Indian Health Service, and Federal Bureau of Prisons; indirectly through other federally sponsored health insurance programs, notably Medicare and Medicaid; and, more broadly through its oversight and other involvement with private sector health insurance plans.
There is no denying that the federal government is a significant participant in the health care system. In the aforementioned contexts, the government generally seeks the legal right to use a patented product (e.g., a medicine or medical device) at a specified purchase price. But federal law provides a mechanism for the government to procure patented products and services without a specific authorization, license, or consent. Further, federal law allows it to use patents without prior consent (this is the quintessential definition of infringement), under limited circumstances, in exchange for compensation to the patent holder. Advocates argue that the federal government should now broadly and unprecedentedly employ this procurement power to combat high drug prices.
Congress’ Enactment of Section 1498(a)
In the early 1900s, Congress enacted legislation permitting the federal government to use patented products without the permission of the rights holder in exchange for some compensation. The statute, § 1498, states:
Whenever an invention described in and covered by a patent of the United States is used or manufactured by or for the United States without license of the owner thereof or lawful right to use or manufacture the same, the owner’s remedy shall be by action against the United States in the United States Court of Federal Claims for the recovery of his reasonable and entire compensation for such use and manufacture.
28 U.S.C. § 1498(a) (emphasis added).
Congress enacted this law (and its subsequent amendments) in response to a number of war time and national security needs, which required the government and its federal contractors to use the inventions of recalcitrant patent owners. In essence, § 1498(a) is a waiver of the federal government’s historic sovereign immunity (hence allowing for lawsuits against the government) while ensuring that the patent owners receive fair compensation. As the statute currently reads, this government intervention is offset by promising “reasonable and entire compensation for such use and manufacture.”
Section 1498 emerged as a solution to a technical standing problem that was preventing IP owners from suing the government for infringement (going back into the 1800s) without reverting to legal fictions such as implied contract. It did not arise simply as strong-arm takings power to benefit the government and contractors. Rather, it is a careful compromise to provide a clear path forward for IP owners while freeing the government from the threats of litigation, such as injunctive relief. While any government intervention in the marketplace must be viewed with some suspicion, the statute ensures that the government will recognize the contribution of innovators through some form of compensation (e.g., an ex post facto royalty).
Scholars conclude that that the statute’s original purpose was to allow the federal government and contractors more flexibility in activities during war time efforts[4]—for example, the government’s procurement of the parts necessary for military equipment or naval ship building. The statute has been used in very few other categories. The Supreme Court observed:
The intention and purpose of Congress in the Act of 1918 was to stimulate contractors to furnish what was needed for the War, without fear of becoming liable themselves for infringements to inventors or the owners or assignees of patents. The letter of the Assistant Secretary of the Navy, upon which the Act of 1918 was passed, leaves no doubt that this was the occasion for it.
Richmond Screw Anchor Co. v. United States, 275 U.S. 331, 345 (1928).
The law and literature reveals two important aspects about § 1498(a). First, it was intended for the government’s limited use of a certain category of patented inventors while respecting their innovative contribution with compensation for their efforts. Rather than civilian inventions, the § 1498(a) case law presents a theme: a series of military, war time, and post-war research related inventions, including weapons, communications equipment involving the Signal Corps of the Army, to stealth airplane carbon fiber fighter plane panels.[5] Second, it was intended as a war time safety valve against recalcitrant inventors – essentially, as a national defense provision. It has been used rarely and in limited contexts. Even when the nation faced an anthrax attack scare, its use was threatened by then HHS Secretary Tommy Thompson, but never actually used.[6] Moreover, it is not a price control mechanism. Nowhere in the text of the statute, the legislative history, nor Supreme Court case law endorses § 1498 as a discount federal procurement mechanism. In other words, § 1498(a) is not a “Groupon” for discounted federal shopping sprees.
Even those advocating for the use § 1498 as a discount procurement tool note a number of potential problems, which include the likelihood of undercompensating innovators and undermining pharmaceutical firms’ incentives to innovate, the potential overuse by the federal government, and giving too much responsibility and discretion to courts to make decisions in this category. Critics of the statute’s use in this context observe that as with any government intervention in the marketplace, consequently, it has a number of negative effects—e.g., chilling innovation, more uncertainty around R&D. The issue about preserving the incentives for R&D for new cutting-edge medicines is not abstract. A Tufts University center study reports that, on average, more than $2.6 billion is spent on R&D for a new prescription drug that gains market approval; the life-cycle cost rises to $2.9 billion when other post-approval develop costs are included.[7] In practice, for every drug that is successfully developed, reviewed, and made available to patients, many dozens more fail.[8] Due to this high failure rate and the costly investment in R&D, well-balanced intellectual property rights are essential for innovators to commercialize the products that do make it to market and improve—or even save—patients’ lives.
In practice, the use of § 1498(a) raises a number of other challenges. The application of a “reasonable royalty” itself leads to uncertainty and lengthy dispute settlement time frames. Ultimately, the retroactive decision of whatever truly is a “reasonable royalty” requires a heightened reliance on the courts to determine its “reasonableness.” The opponents note that this undermines certainty and chills the incentives for innovation. Also, the limited scope of the government’s direct applicability (e.g., prisons, Indian tribes) questions whether this makes its use either an ineffective solution for the public at-large or it will distort markets further by the misallocation of costs on different communities.
Notwithstanding its poor legal mooring for this purpose, in the end, § 1498 is an impractical tool for lowering drug pricing nationwide, vis-à-vis, the widespread government procurement of medicines in the national health care marketplace. As a general proposition, every fundamental understanding of government and liberty informs us that the federal government cannot just seize one’s property—house, livestock, vehicles—for free. Nor can the government use patented inventions (IP) for free.
Conclusion
Today, the Nation faces an increasing populist hue and cry surrounding a number of public health challenges, including the availability and affordability of patented pharmaceuticals. As the cost of drugs sharply rises, outpacing the rate of inflation, policy-makers consider a range of public policy options. The use of a compulsory license or the § 1498 statute offers a superficial false hope/promise to reduce health care spending. Hence, it is naïve to suggest that the government procurement process is designed to give short shrift to inventors by depriving them of just compensation.
Nothing in the § 1498 statute’s wording, history, nor congressionally-mandated purpose supports its role as either a general procurement or price control tool. As with all government interventions into the market place, it has potential consequences. In this context, the consequences are ultimately harmful, e.g., threatening to harm future medical innovation by reducing the incentives for R&D and creating uncertainty in the marketplace. While the goals at the heart of this debate are quite worthy (i.e., increased drug availability and affordability), policy-makers should consider other measures that avoid the inevitable negative consequences. The federal government has an alternate, powerful array of tools at its disposal to improve the access and quality for health care. In sum, § 1498 was never contemplated to be a general procurement discount vehicle—hence the federal government should not begin mistakenly prescribing it.
[1] https://www.trade.gov/topmarkets/pdf/Pharmaceuticals_Executive_Summary.pdf.
[2] The federal government purchases hundreds of billions of dollars of goods and services annually through an array of intricate procurement procedures and systems. These systems are based on willing sellers who work within the government framework (e.g., the schedules also known as Federal Supply Schedules and the Multiple Award Schedules (MAS)) to ensure fairness and a level playing field with pre-negotiated prices rather than letting the federal government use patented products without compensation. See generally https://www.gsa.gov/buying-selling/purchasing-programs/gsa-schedules.
[3] https://www.taxpolicycenter.org/briefing-book/how-much-does-federal-government-spend-health-care (The break down includes spending Medicare ($583 billion), the Medicaid and Children’s Health Insurance Program (CHIP) ($399 billion), and veteran’s medical ($70 billion)).
[4] Sean M. O’Connor, Taking, Tort, or Crown Right? The Confused Early History of Government Patent Policy, 12 J. Marshall Rev. Intell. Prop. L. 145-204 (2012).
[5] Id. at 190.
[6] “Thompson Negotiating With Drug Companies to Purchase Anthrax Antibiotics; Sees No Need to Override Cipro Patent,” June 11, 2009 (“Tony Jewell, an HHS spokesperson, said that agency officials ‘do not believe’ that breaking the patent is necessary, adding, ‘It would not save money to break the patent.'” https://khn.org/morning-breakout/dr00007586/.
[7] https://www.scientificamerican.com/article/cost-to-develop-new-pharmaceutical-drug-now-exceeds-2-5b/.
[8] “The overall attrition rate for new drugs remains high—‘horrendously high’ according to [U.S.] NIH Director Francis Collins—and may be increasing. Recent estimates place the phase 2 failure rate at sixty-five to seventy percent and even higher for drugs with new mechanisms of action.” Erika Lietzan, The Drug Innovation Paradox, 83 Missouri Law Review 39 at 78-79 (2018) (describing the U.S. regime).
 Innovation is all around us. We love and appreciate the latest video games, software apps, and smartphones. We await the integration of self-driving cars and other forms of artificial intelligence. Beyond the gadgets and luxuries we think we can’t live without, there are even more essential products that affect the lives of millions around the world on a daily basis. Patented medicines are at the top of the list of innovations that save lives and preserve the quality of life. Unfortunately, some proposed changes to European patent law are jeopardizing the development and delivery of safe and effective drugs, threatening jobs and innovation, and putting global public health at risk.
Innovation is all around us. We love and appreciate the latest video games, software apps, and smartphones. We await the integration of self-driving cars and other forms of artificial intelligence. Beyond the gadgets and luxuries we think we can’t live without, there are even more essential products that affect the lives of millions around the world on a daily basis. Patented medicines are at the top of the list of innovations that save lives and preserve the quality of life. Unfortunately, some proposed changes to European patent law are jeopardizing the development and delivery of safe and effective drugs, threatening jobs and innovation, and putting global public health at risk.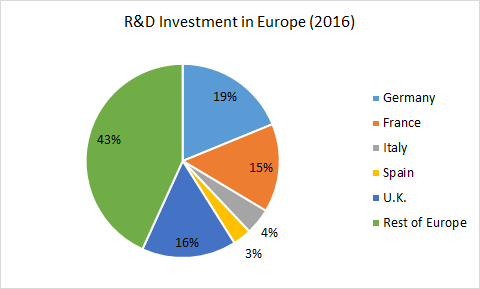
 This past Tuesday, CPIP and the
This past Tuesday, CPIP and the  This drinking water crisis disproportionately affects the poor in the developing world. However, problems with access to safe drinking water may arise in any part of the world due to man-made or natural disasters—including in the United States. One recent example is the
This drinking water crisis disproportionately affects the poor in the developing world. However, problems with access to safe drinking water may arise in any part of the world due to man-made or natural disasters—including in the United States. One recent example is the  The pesticide removal technology developed by Dr. Pradeep and his colleagues works by utilizing the ability of
The pesticide removal technology developed by Dr. Pradeep and his colleagues works by utilizing the ability of 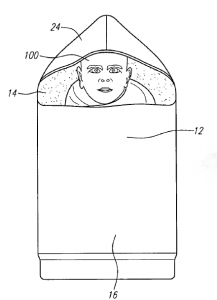 Specifically, there has been a need to design infant incubators that address the unique challenges of the developing world.
Specifically, there has been a need to design infant incubators that address the unique challenges of the developing world. 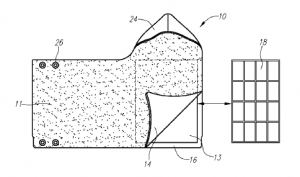 These materials are called “phase change materials” because they melt or solidify (in other words, they change phases) near body temperature. People normally think about the transfer of heat energy as making one thing warmer or another thing colder, but this is not true during a phase change. For example, during solidification, the material releases heat energy, which can be used to keep the infant warm, but it maintains its own temperature because the heat comes from the process of solidification rather than a loss of temperature.
These materials are called “phase change materials” because they melt or solidify (in other words, they change phases) near body temperature. People normally think about the transfer of heat energy as making one thing warmer or another thing colder, but this is not true during a phase change. For example, during solidification, the material releases heat energy, which can be used to keep the infant warm, but it maintains its own temperature because the heat comes from the process of solidification rather than a loss of temperature.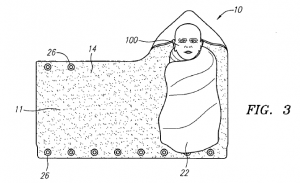 To further advance their invention, the team founded the Embrace Innovations company and have begun developing a strong
To further advance their invention, the team founded the Embrace Innovations company and have begun developing a strong  Miriam achieves its goals through a
Miriam achieves its goals through a